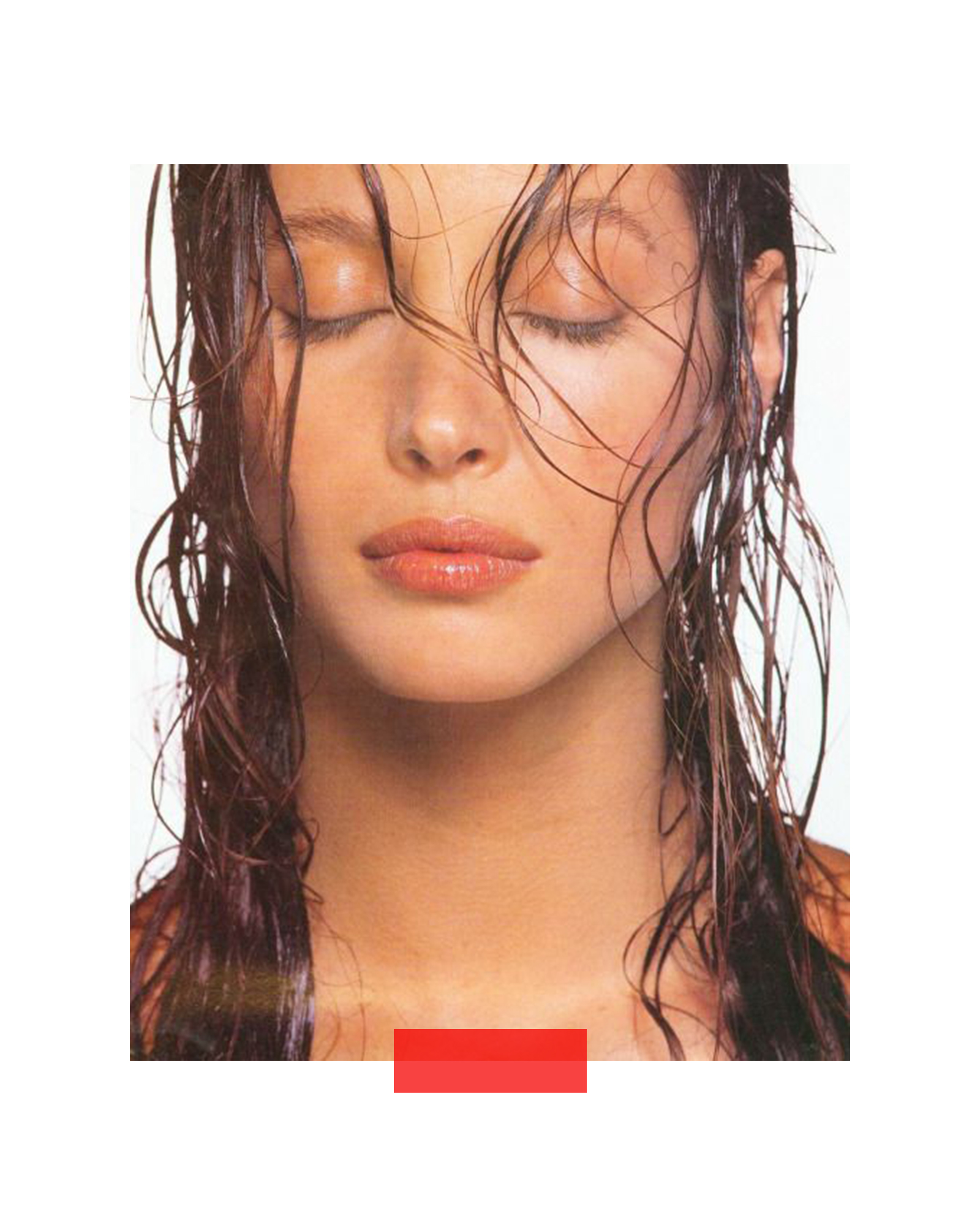
Milia are common, benign skin conditions characterised by the presence of small, firm, white or yellowish bumps that appear on the skin's surface. These are not a form of acne, nor are they caused by clogged pores in the same way as blackheads or whiteheads. Instead, milia are tiny cysts filled with keratin, a naturally occurring protein found in skin, hair, and nails, which becomes trapped just beneath the skin's surface. They are typically found around the eyes, cheeks, nose, and forehead, but can appear anywhere on the face or body. While harmless and not contagious, their presence can be cosmetically bothersome for many individuals.
Types and Causes of Milia
Milia can generally be categorised into a few types based on their cause and onset:
- Primary Milia: These develop spontaneously, often with no clear preceding cause. They are common in newborns (known as neonatal milia or "milk spots"), where they usually resolve on their own within a few weeks. Primary milia can also occur in children and adults, sometimes persisting indefinitely if left untreated.
- Secondary Milia (Traumatic Milia): These develop after some form of skin trauma or damage, such as burns, blistering rashes (like poison ivy), prolonged sun exposure, skin grafting, dermabrasion, or radiotherapy. They form as the skin heals and dead skin cells become trapped.
- Milia En Plaque: A rarer type, usually affecting women between 40 and 60, where milia cluster together on a raised, often erythematous (red) plaque, typically behind the ears, on the eyelid, cheek, or jaw.
- Juvenile Milia: These are milia that occur as a symptom of certain inherited genetic skin conditions (genodermatoses).
- Medication-Induced Milia: Prolonged use of certain medications, particularly topical steroid creams or ointments, can sometimes lead to milia formation.
The underlying mechanism involves a failure of the skin to naturally shed dead skin cells (keratinocytes) from its surface. Instead, these cells become entrapped within small pockets just below the epidermis, forming the characteristic hard, pearly white bumps.
Treating Milia
It is crucial to understand that milia cannot be squeezed or "popped" like a pimple. Attempting to extract them at home can cause damage, irritation, infection, or even scarring, as there is no open pore or pus to express. Professional intervention is generally recommended for effective and safe removal.
Professional Treatment Options:
- Manual Extraction (De-roofing): This is the most common and effective method. A trained aesthetician or dermatologist uses a sterile, fine needle or lancet to create a tiny incision on the surface of the milium and then gently extracts the trapped keratin plug. This should only be performed by a qualified professional in a sterile environment.
- Cryotherapy: Involves freezing the milia with liquid nitrogen, causing them to blister and eventually fall off. Not always recommended for sensitive areas like around the eyes.
- Diathermy/Electrocautery: Uses heat to destroy the milia.
- Laser Ablation: A laser can be used to open and destroy the milia.
- Chemical Peels/Microdermabrasion: While not directly removing existing milia, regular treatments can help to promote overall cell turnover and prevent new milia from forming, and may help existing ones surface over time.
At-Home Management & Prevention:
While direct removal of existing milia is best left to professionals, a consistent skincare routine can help prevent new milia formation and may, over time, encourage some superficial milia to resolve.
- Gentle Cleansing: Use a mild, non-stripping cleanser daily to keep the skin clean and help prevent the buildup of dead skin cells.
- Regular, Gentle Exfoliation: This is key. Incorporate chemical exfoliants such as:
- Alpha Hydroxy Acids (AHAs) like glycolic acid or lactic acid: These work on the skin's surface to help shed dead skin cells.
- Beta Hydroxy Acids (BHAs) like salicylic acid: These are oil-soluble and can penetrate deeper into pores, helping to dislodge trapped keratin.
- Caution: Avoid over-exfoliating, which can irritate the skin and potentially worsen the condition.
- Topical Retinoids: Over-the-counter retinol or prescription retinoids (e.g., tretinoin, adapalene) encourage faster cell turnover, which helps prevent keratin from becoming trapped. Introduce these slowly to minimise irritation.
- Lightweight Moisturisers & Eye Creams: Avoid excessively rich or heavy creams, particularly around the delicate eye area, as these can contribute to keratin trapping. Opt for lighter, non-comedogenic formulas.
- Sun Protection: Diligent daily use of a broad-spectrum SPF 30+ (or 50+) sunscreen is vital. Sun damage can thicken the skin and impede its natural exfoliation process, contributing to milia formation.
- Avoid Self-Extraction: Resist the temptation to pick or squeeze milia. This is ineffective and can lead to inflammation, infection, and scarring.
If milia are persistent, widespread, or causing significant cosmetic concern, consulting a dermatologist is always recommended for an accurate diagnosis and a tailored treatment plan.